Brittany Taylor is a biomedical engineer and assistant professor who studies novel ways to improve bone and tendon healing after injuries. She is exploring drug delivery systems and temporary artificial tissue replacements to promote healing of tendons and the interface with bones and muscle. Millions of musculoskeletal injuries each year cause pain and reduce people’s quality of life. Here, she answers questions about the benefits of using composite materials – biological materials like tissue from animals or synthetic materials – to improve repair outcomes. Many of the techniques are still in the experimental stages and have been tested in animal models.
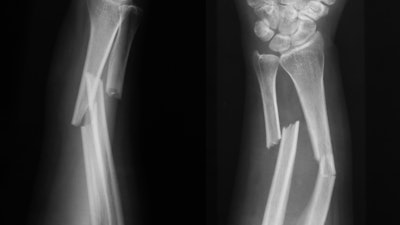
At least half a million bone grafts a year are performed in the United States. Why do doctors and patients need an alternative to using real bone in these surgeries?
Musculoskeletal complications due to disease, traumatic injury or repetitive activity are major problems worldwide. Current treatments to repair these injuries rely on harvested or donated tissue. For example, doctors take bone from the iliac crest, the curved portion at the top of the hip, then mold it to fit the area needing the bone replacement. But donation sites for bone are limited, and there is a risk of tissue death where the bone is extracted.
When another patient or a cadaver provides bone for such repairs, it can transmit disease. Harsh detergents and sterilization methods to remove any disease can also affect the bone’s strength.
The use of composite material overcomes the risks and problems of real bone.
What kinds of materials work best to help injured bones regenerate?
Composite materials that have a combination of metals, ceramics and polymers – human-made substances – appear to work best for bone regeneration. They provide mechanical support and also a matrix for tissue development. Biomaterials – engineered materials designed to interact with real body tissue – can regenerate tissues and help healing.
The biomaterial should be compatible with the body. It should not set off an immune response, and it should match tissue’s structural and mechanical properties. Biomaterials used for bone tissue engineering should be as tough as bone and allow for tissue to grow into the structure. Natural materials such as collagen from cows or pigs can also be integrated into the bone scaffold to promote bone repair.
You study tendons and their limited ability to regenerate when torn. Why don’t tendons heal themselves easily?
Tendons do not regenerate well because they have low cellularity – fewer clusters of cells than other parts of the body – and fewer blood vessels. Tendons also form scar tissue as they heal and therefore have limited functionality. Surgically repaired tendons can also easily retear, which reduces a person’s quality of life and lead to prolonged complications. Therefore, researchers are working on tissue engineering strategies to augment healing.
What kind of engineered materials can help tendons heal?
Tendons are fibrous tissues that transmit energy loads from muscles to bones. They are “highly aligned,” which means they orient along the direction of the load they transmit. Any engineered biomaterial that replaces a tendon should mimic its mechanical force and allow cells to attach and grow on them, as real tendons do. Therefore, polymer-based biomaterials are the best materials to engineer tendon tissue. Engineers make the experimental polymers with techniques such as electrospinning, which uses an electric field to draw a nanosized polymer strand from a solution, making nanofibers.
Nanofibers can be combined with other materials to engineer tendons, as they have a large surface area-to-volume ratio and are porous. Cells easily adhere to these materials.
You have worked on developing stronger scaffolds that act like real bone in the body. What do scaffolds do, and why do they need to be made stronger?
Biomaterial scaffolds for tissue engineering are similar to scaffolding used in construction: a temporary framework that supports the structure and provides a platform for the builders to climb and place materials in their appropriate location. Once the construction is complete, the scaffolding is removed and the newly built structure remains.
The same process works in the human body. Cells attach to the scaffold, proliferate and migrate throughout the scaffold. As the cells “climb” they start to deposit biological factors that promote tissue formation.
The scaffold degrades over time as the new tissue regenerates. Mechanical supports can be added to the scaffolds to make them stronger. My colleagues and I included ceramic posts made out of naturally occurring bone mineral, hydroxyapatite, in the three-dimensional composite bone scaffold for load-bearing applications. The posts were similar to beams added to a structure.
As a Black scientist, you have advocated for good mentors to help other scientists of color.
I have had to overcome several societal and academic challenges. As a Black first-generation college graduate and female biomedical engineer, I am underrepresented at every level of academia. The obstacles I conquered and the knowledge I gained along this journey contribute to the diverse perspective I bring to the field as a culturally competent educator, well-rounded scientist and strong mentor.
My vision for diversifying scientific research is to continually influence members of the next generation as they work their way through their studies. I mentor scientists, transparently share my experiences and encourage trainees from all backgrounds.
I strongly believe a significant part of being successful in academia is the ability to mentor and be mentored throughout the academic pipeline. I am grateful for the many mentors throughout my journey who opened doors for new opportunities and provided access to the necessary spaces to get me to where I am now. And I am committed to doing the same for others.
This article is republished from The Conversation under a Creative Commons license. Read the original article here: https://theconversation.com/the-promise-of-repairing-bones-and-tendons-with-human-made-materials-170076.






















